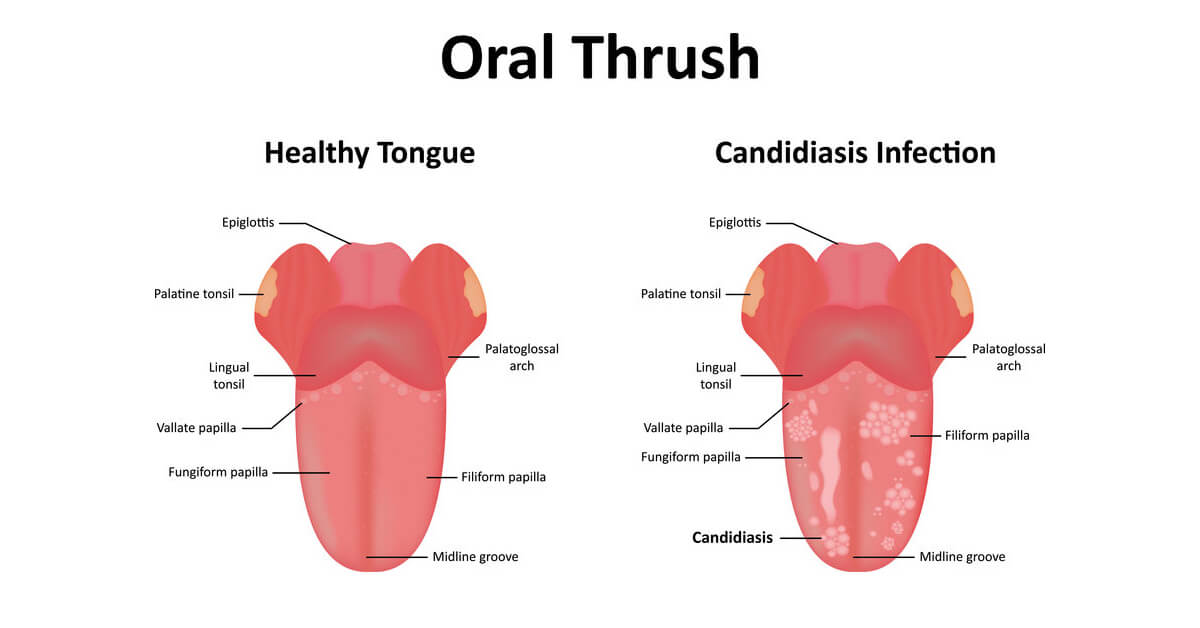
Oral thrush (candidiasis) is a common fungal infection. It presents as a red, sore and sometimes white lesion in the mouth.
If you have oral candidiasis, a natural remedy may be oral probiotics.
Oral probiotics work by replacing essential bacteria in your oral flora. This restores the balance in your oral microbiome. Fungal infection indicates your oral microbiome is out of balance.
Very few doctors recommend oral probiotics to treat oral thrush. Research shows the most common treatment for oral thrush is medication. One study showed that 30% of physicians prescribe Nystatin for oral thrush in infants without even examining them.
Medication will usually cure thrush, even if only for a while. However, it’s often prescribed with little thought for why thrush has occurred – or how it may be prevented. This is an oversight, because oral thrush may be a sign of other problems in your body. Also, an imbalance in your oral microbiome can cause many other health problems.
In this article, we will explore why oral thrush occurs. You will also see how oral probiotics could improve your overall health.
What Is Oral Thrush?
I see many patients with oral thrush. Many of them don’t know they have a fungal infection in their mouth.
Oral thrush is caused by the fungal species Candida albicans.
Common signs you have an oral thrush infection are:
- Cracking or redness on corners of the mouth (angular chelates).
- Red, sore lesions or blisters.
- Creamy white bumps or ‘cottage cheese’ lesions on the tongue or inner cheeks.
- White covering on the roof of your mouth, gums, tonsils or back of the throat.
- ‘Cotton’ feeling in the mouth.
- Loss of taste.
- Difficulty swallowing.
- Bad breath.
Often, it’s a mild infection without major complications. Red cracked lesions on the corners of your lips are a common sign of mild thrush. However, oral thrush can sometimes become severe.
Let’s look at what oral thrush means for your oral microbiome.
Can oral thrush tell us about yeast infection in the body?
Fungal infection or thrush is a common problem throughout the body. In the mouth, thrush is easily identified. But it’s important to know whether you have a fungal infection elsewhere.
Here are some common sites of fungal infection:
Skin
Fungal infection can occur in the armpits, groin, fingernails, toenails or under the breasts. It presents as red, bumpy or white lesions hiding under a fold of skin.
Vagina/penis
Vaginal or penile thrush may present with a white to yellow discharge. It can be uncomfortable, itchy and cause pain when urinating.
Throat, tonsils, and windpipe
Thrush of the throat and windpipe can be a sign of serious disease. It is often seen in patients suffering from AIDS. It can cause chest pain, nausea, and pain on swallowing.
Systemic candidiasis
A fungal infection throughout the body can be life threatening. It can affect your eyes, liver, genital tract, joint, brain, kidney, and heart. It’s most common in people with severe immune system depression.
Symptoms of candida infection elsewhere in your body include:
- Fatigue
- Cravings for sweets
- Brain fog
- Joint pain
- Loss of sex drive
- Chronic sinus and allergy issues
- Digestive problems (gas and bloating)
- Frequent sickness
- UTI
These symptoms may exist alongside oral thrush. If you experience any of these, you should consult your physician.
Oral thrush and fungal infection is an immune problem
If you have oral thrush, your body is sending you signals. It’s telling you your immune system isn’t coping well. It’s also a sign of microbiome ‘dysbiosis’ (imbalance).
Oral candidiasis is most common in elderly people and those with conditions that weaken the immune system.
You are at highest risk of oral thrush if you:
- Have recently taken antibiotics, particularly a long course or high dose.
- Are taking steroid medication (often for asthma).
- Are taking the oral contraceptive pill.
- Have iron or vitamin B12 deficiency.
- Wear dentures (false teeth), particularly if they don’t fit well.
- Have poor oral hygiene.
- Have a dry mouth, either because of a medical condition or a medication.
- Are a smoker.
- Are having chemotherapy or radiotherapy to treat cancer.
- Have HIV.
Oral thrush is commonly treated with an anti-fungal medication such as Nystatin or Fluconazole. These may be in a liquid, lozenge, tablet, capsule or topical cream form.
Medication and treatment of oral and systemic thrush
Oral thrush is commonly treated with an anti-fungal medication such as Nystatin or Fluconazole in a liquid or lozenge form. Tablets, capsules or a topical anti-fungal cream may also be prescribed.
Usually, topical medication is applied for 7 to 14 days. Tablets or capsules are usually taken once daily.
Nystatin and Fluconazole target the wall of a fungus cell, causing them to leak and die. They are both effective for treating oral thrush.
However, they both have broad anti-fungal effects. This means they also remove beneficial fungus from the oral microbiome.
Fungus and yeast in the oral microbiome
The ‘human microbiome’ is the microbial environment in your body. The ‘mycobiome’ refers to the fungal communities within it. Much less is known about the fungal species in your body than the bacterial species.
How many fungal species live in the oral microbiome? We’re not sure yet.
We do know that Candida lives in the healthy microbiome, so it’s mere presence doesn’t indicate thrush infection. However, we know little about healthy levels of yeast and fungi. This is why anti-fungal medications may do harm while trying to do good.
They also don’t address the cause of thrush. That’s why using oral probiotics could be a good alternative.
Is candida part of a healthy microbiome?
Oral thrush is a condition that has a high re-occurrence rate. This may be due to using anti-fungal medications alone. They may remove oral thrush, but don’t address its root cause – so it returns.
As with other oral diseases, oral thrush suggests microbiome dysbiosis (microbial imbalance).
Candida is one of over 700 species living in the oral microbiome. But fungal populations in the mouth vary greatly from person to person.
Yeast is a highly resilient species of microbes. When we acquire them from birth, they stick around. But little is known about what fungi actually do in your body.
Diet as a cause for microbiome imbalance
In your oral microbiome, probiotic bacteria help to maintain a healthy mouth. So, when you don’t ‘feed’ them, imbalances occur.
A diet high in processed foods and sugars favors certain bacteria. These fast metabolizing bugs overgrow – and outgrow your probiotics. This is how oral dysbiosis results in tooth decay and gum disease.
But oral dysbiosis is also related to candida overgrowth. In oral thrush, candida builds up and binds to your gum surface. There, it forms white patches like dental plaque. Normally, probiotic bacteria stop candida from building these plaques.
Researchers are still to understand the precise connection. However, we know that oral flora imbalance is the first step in gum disease and oral thrush. Similarly, both diseases are related to immune dysfunction.
Can oral probiotics cure candida?
Probiotics release substances that stop the growth of harmful species.
Lactobacilli species release lactic acid that inhibits candida growth. The organic acid seems to shut down candida energy systems. This is a natural defense against the overgrowth of candida. So oral thrush signals a loss of oral probiotic populations.
Does research support oral probiotics as a treatment for candida?
So, what does research say about the benefits of oral probiotics? Does it support oral probiotics against oral Candida?
In the elderly, oral thrush is common. This is due to medications and compromised immunity. One large study compared elderly patients eating 50g cheese with added lactobacilli probiotics with a control group eating normal cheese. The probiotic cheese had a positive effect on oral candida. Researchers found a decreased yeast count as well as lower saliva levels.
In another study, children ate cheese containing L. rhamnosus. This showed a decrease in salivary yeast and mutans, a bacteria species that causes tooth decay.
The efficacy of oral probiotics against oral thrush was studied in elderly denture wearers. Elderly denture wearers are at high risk of oral thrush. A high-quality study tested the benefits L. rhamnosus, L. acidophilus, and B. bifid probiotic species together. Results showed that multiple probiotic species could prevent candida in high-risk groups.
Another randomized control trial used probiotic lozenges. The probiotics containing two strains of L. rhetoric was tested on frail elderly people in nursing homes. The probiotic lozenges reduced high Candida counts in subjects.
S. salivarious inhibits disease-causing bacteria. It’s thought to help prevent bad breath and tooth decay. However, research has also found broad broader benefits of K12 against oral Candida.
Gut probiotics, prebiotics as synbiotics
The benefits of taking oral probiotics to prevent or cure candida require more study. Probiotic research has focused more on the benefits for gut health. And this may also benefit oral thrush.
One study looking at probiotic yogurt with L. casei and B. breve on concluded it had positive benefits in oral candida cases. The probiotic yogurt boosted levels of IgA antibodies that fight candida.
Probiotics may act by helping immune system regulation in the gut. In the gut, the immune system and gut microbes work together. They form antibodies and coordinate the immune response. The oral microbiome is also involved in the immune response. Oral probiotics may help there too, as well as maintaining bacterial balance.
Oral prebiotics are non-digestible fibers. They may also be effective against oral thrush in two ways.
Firstly, they feed friendly probiotic bacteria. This is called a synbiotic action. Very little is known about oral symbiotic and what they do in the mouth.
Secondly, oral prebiotics are similar to dietary fiber. They may increase bacteria that release enzymes to break down candida’s fibrous cell wall.
The action of prebiotics and symbiotic probiotic against candida is an area worthy of further research.
The Verdict: Can oral prebiotics cure oral thrush?
Oral thrush indicates a weakened immune system and microbiome imbalance. You may need anti-fungal medications to cure your oral thrush. However, restoring oral microbiome balance should be your long-term goal.
Research supports the benefits of oral probiotics against oral Candida. However, so far trials have been mostly limited to elderly and immune compromised patients. Oral prebiotics, symbiotic and dietary changes may also be helpful.
If you have oral thrush, you should consider:
- Reducing intake of sugars and processed carbs.
- Increasing dietary fiber and vegetable intake.
- Taking an oral probiotic containing the species rhamnosus, L. acidophilus, and B. bifid
- Consulting your physician if you have symptoms of systemic candida infection.
Do you have any questions regarding oral thrush? Ask them in the comment section below.
For more information on Dr. Lin’s clinical protocol that highlights the steps parents can take to prevent dental problems in their children: Click here.
Want to know more? Dr Steven Lin’s book, The Dental Diet, is available to order today. An exploration of ancestral medicine, the human microbiome and epigenetics it’s a complete guide to the mouth-body connection. Take the journey and the 40-day delicious food program for life-changing oral and whole health.
Click below to order your copy now:
US AMAZON
US Barnes & Noble
UK AMAZON
Australia BOOKTOPIA
Canada INDIGO




10 Responses
Is it ok to take probiotics & prebiotic while taking oral Nystatin?
Check drug interractions on the packaging.
Try taking at different times in the day.
Thank you for posting this great information. I have had great results treating oral thrush by consuming fermented foods such as kefir. I was hoping to find some info to back the benefits of probiotics and yeast growth prevention so I could share this with my patients.
42 Year old woman who had sinus surgery (FESS) in October 2017. I have been raspy in the voice since. I took about 6 weeks worth of antibiotics prior to surgery trying to fix the issue. I also do a Advocare 10 day cleanse every 90 to 180 days. Could this be a cause of developing oral thrush. I had an immune test done prior to surgery as well, just to rule that out as an issue for the reoccurring sinus infection. I was wondering is I should start an oral probiotic to help assist in the healing? I have been dealing with this for about 6 days and on a second round of treatment.
I got a mild case of oral thrush after taking multiple rounds of antibiotics. My doctor prescribed clomzole lozenges. I also took probiotics, gargled with salt water, alcohol free mouthwash, flossed two times a day, and used a hydrogen peroxide based tooth whitener in tooth whitening trays. Therabreath also makes some great lozenges etc… After two weeks of this I am almost yeast free. One more thing, although my problem was oral, I tried Monostat, hoping that if the infection was systemic, the anti-fungal would address that issue. I’m sure it sounds as if I went overboard but I hate not feeling comfortable with being able to speak and communicate freely. I am 90% better and with time am looking forward to a full recovery. Good luck to you!
Can I ask what probiotic you take? I also got a mild case of oral thrush after antibiotics and would like to find the right one – so many on the market! I just started the lozenges and want to be sure it clears up!
Hi Dawn,
Oral thrush is a sign of lowered immune system, if you were tested, you may have a gut/microbiome imabalance. I would investigate your gut health including vitamin D, sleep health and probiotics may assist re-balance the oral environment
Hope this helps.
Chelsea
Community Manager
http://www.drstevenlin.com
Would changing the mothers diet help treat oral thrush in breastfedbaby?
Hi, I have had oral thrush for a year and a half after taking two rounds of strong antibiotics for an ear infection. I have tried taking probiotics, digestive enzymes, prescribed antifungals, herbal remedies, gentian violet and been on the candida diet for the last 6 weeks. It is finally begining to go with just a few sores left in my mouth but low and behold I have just been prescribed another strong dose of antibiotics for another ear infection. What can I do to make sure it doesn’t come back again tenfold as I seem to have real trouble getting rid of it. (I think my gut is out of balance as I am vit b12, iron, and d deficient after being given numerous rounds of antibiotics for ear infections due to eustachian tube dysfunction) Any help will be gratefully received!!
Candidiasis Herbal Treatment read the Symptoms and Causes. Candidiasis, also called thrush or moniliasis, is a yeast infection. The skin is a fungal infection that causes a red,itchy rash your skin folds.